We know that registrants have stressful jobs and that many have had to fill challenging new roles in response to the pandemic. Sadly, this can take a toll on registrants’ mental health and in some cases lead to registrants experiencing distressing symptoms, including suicidal ideation. Suicidal ideation (or suicidal thoughts) is a broad term and can cover thoughts about wishing you were dead to thinking about taking your own life including planning to take your own life.
At the HCPC, we believe we have an important role to play in ensuring the wellbeing of registrants. We also know that registrant wellbeing is a vital part of ensuring service user safety. Our priority therefore is ensuring that registrants have access to advice and support, so that they can get the help they need and ensure they are able to continue to practise safely, without fear of the impact on their registration. To support this, we have produced online materials aimed at registrants and updated our Guidance on health and character to include more illustrative case studies.
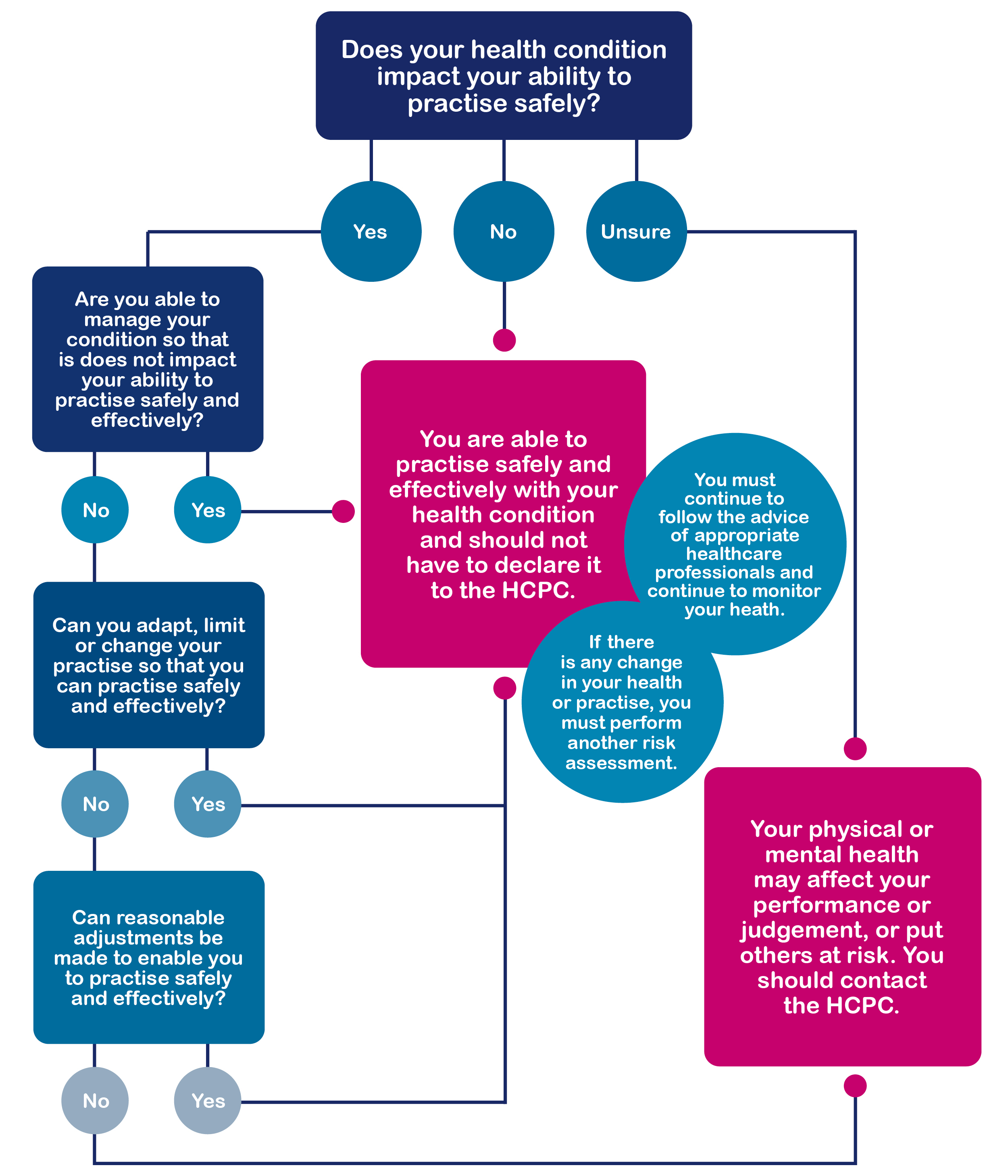
Our guidance on health and character does not contain a list of health conditions which would impact on a professional’s registration. This is because our focus is on the impact of those health conditions on the ability of registrants to practice safely and effectively, as opposed to simply the diagnosis.
In the case of suicidal ideation, this means that simply experiencing this does not mean a registrant must cease practicing or refer themselves to us.
Where a registrant experiences suicidal ideation, this would only raise fitness to practise concerns for the HCPC, and therefore require a referral, if this meant that a registrant was no longer able to practice safely and effectively.
Whenever a registrant has a health concern, we would expect them to seek and follow advice from a relevant healthcare professional and to follow the policies of their employer at all times. Registrants can find more health and wellbeing resources on the HCPC’s website but should also check what resources are available to them through their employer. Remember that you can call Samaritans on 116 123 24 hours a day, while Mind’s specialised service for frontline workers can be reached on 0300 303 5999.
Case study
Like your physical health, your mental health can change. Just like your physical health, it is possible to live with a mental health issue and, through the necessary steps, manage your condition effectively and practise safely.
A registrant has begun experiencing suicidal ideation, following a short period of poor mental health.
The registrant has been seeing an appropriate healthcare professional who helps him manage his mental health. He has been prescribed medication which helps to manage his mental health and he made his employers aware early on.
He began seeing a healthcare professional. Through the advice of this professional and after conversations with his supervisor and with his colleagues, he knows that a trigger for his condition is extreme stress. His employers have put in place several safeguards like allowing him to reduce his working hours and providing time to debrief after challenging cases to ensure that he is able to manage the level of stress associated with his role. Those working closely with him are also informed, with the registrant’s consent, about his condition and the triggers so they can be included in a network of support.
He is unsure about whether he needs to disclose his health condition to the HCPC and if so, when he would need to do this.
He contacts his professional body and they advise him that he seems to be following appropriate healthcare advice, his employer is aware and has placed safeguards in place and that he appears to be appropriately managing his condition. His professional body informed him that if he was still unsure whether or not he needed to make a declaration, then he should contact the HCPC.
If he is sure he can adapt, limit, or stop his practice as needed to remain safe and effective, then he does not need to inform the HCPC. When he was in very poor health, he had stopped working by taking leave and has only begun to work again as his health has improved and since managing his condition. He has been able to adapt his practice as needed in order to remain safe and effective.
If something changes and he can no longer practise safely, he will not be able to meet Standard 6.3 of his Standards of conduct, performance and ethics and should inform the HCPC immediately.
When do I need to report a health condition to the HCPC?